High Dropout Rates Highlight Treatment Challenges
Clinical trials for Kobefi revealed that while some patients experienced beneficial effects with minimal side effects, many participants discontinued treatment before completing the studies. This dropout rate is not uncommon in schizophrenia drug trials, reflecting the difficulties patients face in sticking to treatment plans. Factors such as the burdensome side effects of existing medications—including weight gain, tremors, and restlessness—often lead individuals to stop taking their prescribed drugs, resulting in the recurrence of symptoms.
How Kobefi Works Differently
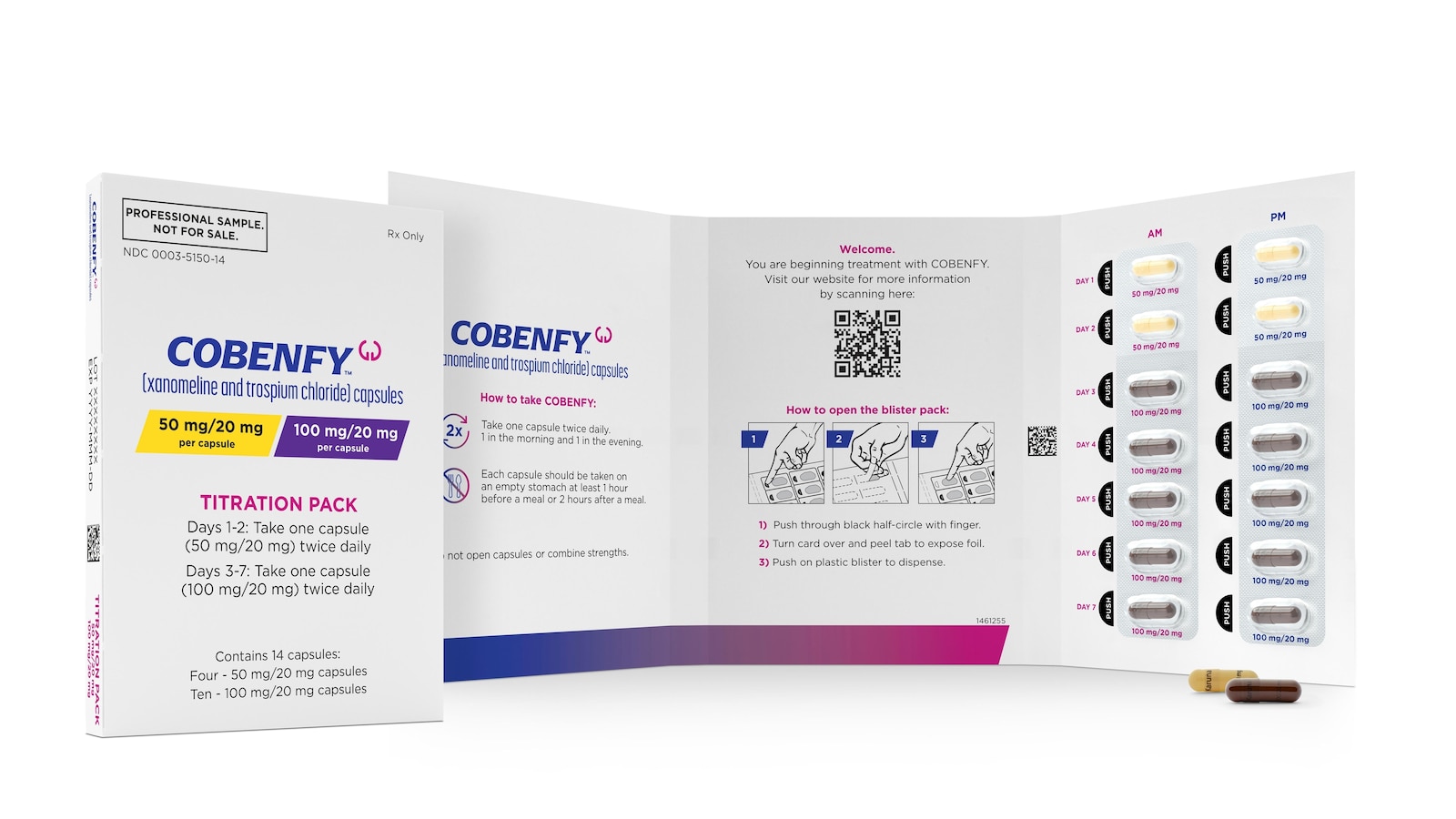
Kobefi, which gained FDA approval in September, is gaining attention because of its unique mechanism of action. Unlike traditional schizophrenia medications that block dopamine receptors, Kobefi’s active component, Xenomeline, targets a different receptor that indirectly inhibits dopamine release. This novel approach aims to reduce the typical side effects associated with schizophrenia treatments. Additionally, Kobefi contains Trospium, which is believed to mitigate some common side effects such as nausea, vomiting, and gastrointestinal discomfort. In a positive contrast to other antipsychotics, patients taking Kobefi reported losing a few pounds instead of gaining weight.
Promising Results Amidst Study Dropouts
Dr. John Krystal from Yale University, who has led research on other schizophrenia medications but was not involved in the new studies, noted that the dropout rate—where 78% of severely ill patients left one study and 51% from another—parallels what is typically observed in such trials. However, he highlighted that among those who completed the studies, 69% of the severely ill group experienced significant symptom improvement by the year’s end, compared to 30% in the more stable group.
Understanding Patient Retention in Trials
As researchers continue to analyze the reasons behind the high dropout rates, Dr. Krystal emphasized the importance of understanding patient experiences and treatment adherence. Encouragingly, follow-up interviews with study participants revealed that 36 individuals expressed interest in continuing Kobefi if given the opportunity, while only 10 opted out. Some patients noted a decrease in auditory hallucinations, although others reported minimal benefits.
Cost Considerations and Future Accessibility
While Kobefi presents an exciting advancement in schizophrenia treatment, its estimated annual cost of $22,500 raises concerns about accessibility. In contrast, generic antipsychotics can be obtained for as little as $540 annually. There is apprehension among experts that insurers may require patients to first try less expensive medications before covering Kobefi. Most patients’ out-of-pocket expenses are expected to be lower, depending on their insurance plans.
Dr. Krystal pointed out that Clozapine, a widely regarded but underutilized generic medication in the U.S., is considered one of the best treatments for schizophrenia, despite its stringent monitoring requirements due to risks of severe neutropenia. This has resulted in some patients experiencing relapses due to delays or restrictions in accessing Clozapine.
Voices from the Community
Patients and their families are eager for more information regarding the real-world effectiveness of Kobefi. Sally Littlefield, a 29-year-old resident of Alameda, California, who suffers from schizophrenia and bipolar disorder, expressed a desire to learn more about the experiences of those who have taken Kobefi beyond just the financial implications. Meanwhile, Mindy Greiling from Roseville, Minnesota, wants to see data comparing Kobefi with Clozapine, which has proven effective for her son, Jim. Greiling mentioned that concerns about weight gain were alleviated once her son began medication for diabetes.
As Kobefi garners attention for its innovative approach, patients, families, and healthcare professionals alike are watching closely for further studies and data that will elucidate its long-term effectiveness compared to existing treatments like Clozapine.